


It feels like it’s been so long since my last update but it’s only been a little over a month. When I last wrote an update, I had just started Gonal-F injections since my body hadn’t responded to the estrogen protocol we tried in month 1.
After estrogen pills, patches, trental, vitamin E and baby aspirin failed to increase my lining enough and I never got a trilaminar line in my uterus, my doctor switched me to Gonal-F injections. It’s typically used in egg retrieval cycles (and I was on it when we did my egg retrieval a few years ago) and we were hoping that it would stimulate my uterine lining more than estrogen did.
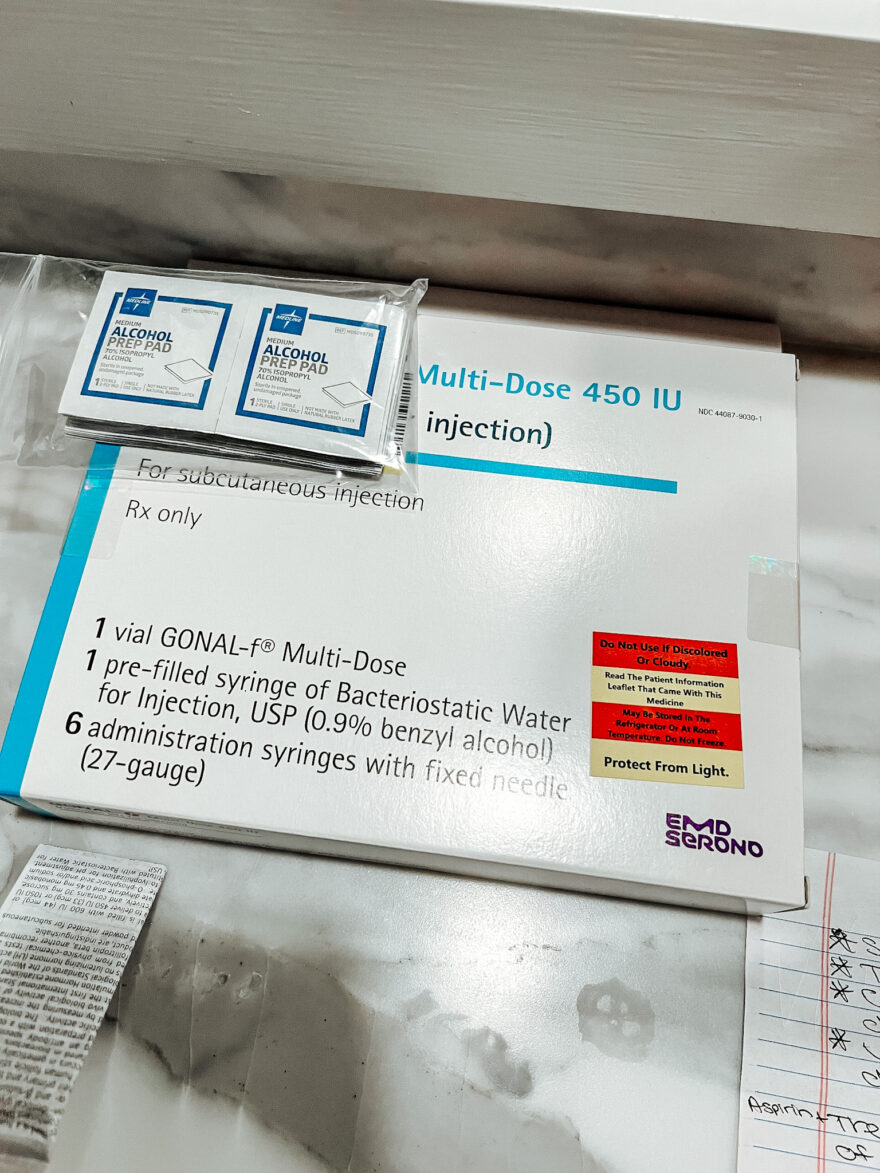
I had bloodwork and an ultrasound on April 3 and then started Gonal-F injections that night, 75 mL once a day. After a few days, I went in for bloodwork on April 6. And there was basically no change, so we bumped up to 112.5 mL. Same thing after a few days – more bloodwork and more measurements and no change. My estrogen had gone up a little but not enough (from 18 to 32) and my lining was still only measuring at 3.7mm. At this appointment, I asked the nurse what we’d do if Gonal didn’t work. She said that PRP injections can increase lining thickness, but to not get too far ahead of myself. Then I left that appointment with instructions to bump up my Gonal dose to 150 mL nightly.
I struggled with postpartum anxiety and depression with suicidal thoughts after I had Thomas. But I hadn’t had issues with that since I got on medication. However, the same dark thoughts came back within a week of being on Gonal-F. I was also crying a lot, which is not my normal. The nurse said that Gonal can cause these problems for those who already have a history with PPDA and that we’d monitor things closely.
On April 10, my lining had gone up to 4.8mm and my estrogen levels had increased (as well as the size of the one follicle I had) but when the doctor was reviewing the results, he instructed the nurse to have me stop Gonal and that we’d do PRP injections next. He said we simply weren’t getting the response we needed (we need to get to at LEAST 8mm), given the high dose I was on. Unless we did something else for my mood (like adjusting my anxiety meds or something), I was nervous to stay on it for much longer. Additionally, the medication is significantly more expensive than estrogen. A 450 mL vial of Gonal-F was around $500. And I was going through a vial every 3 days vs. the $75 monthly cost of estrogen.
What I found frustrating at this point was that the nurse coordinator called me to schedule PRP but no one had explained anything about it to me other than the brief mention by the nurse. The only way I knew what PRP even stood for was because I’d considered it for a torn ankle tendon a few years ago, when I was struggling with a running injury that wouldn’t heal.
When I asked questions, the coordinator couldn’t answer my questions because “we don’t do it that often, so I’m not sure” and had to go ask the doctor. I asked if I could just schedule an appointment with my doctor to discuss the plan for my care and was told no. They won’t let me schedule an appointment with him. She said I can call his cell phone after hours or do a telehealth visit if I insisted on seeing him.

I’m honestly so baffled by this. I met with the doctor multiple times when we did the egg retrieval a few years ago (which was only a two month process) and now I can’t see him, even after being in their care — without the results we need — for four months. The only thing I can figure out is that the practice size has grown so much between now and then. And he prioritizes time on procedures. I don’t know if I should be understanding or if I am right to be frustrated. I suppose I’ll call his cell phone. But I’d much rather be able to sit down with the doctor and my husband and talk through all my questions and concerns.
It’s enough to make me want to switch practices. But they have one of the highest success rates in the country. And I had a horrible experience with the other fertility clinic in town (Baptist/Atrium) when we were learned about my ovarian failure four years ago.
However, I do have PRP scheduled for next week. PRP stands for platelet-rich plasma and in short, they’ll draw my blood, spin it to separate the plasma out and inject it into my uterine lining. Plasma is high in growth factors, so that’s why it is used to help with lining thickness. Then, we’d hopefully get the thickness we need and a frozen embryo transfer would happen 6-8 weeks later. However, it’s a relatively new procedure for fertility treatment. And I’m curious why we haven’t first tried other protocols that I’ve read about. Perhaps I’m not a candidate for them. But I want to understand why PRP is what my doctor chose as the next step.
Is my case so unusually difficult that he wants to do PRP? Why is it uncommon at their practice, so much that the IVF coordinator didn’t know much about it? I have more questions than answers. And not understanding the recommendations makes it hard for me to trust the plan. And trusting my doctor and the plan is crucially important.
An additional layer that I was trying to figure out was when to go home to see my family in Utah. I had postponed the trip for months because of fertility treatments. I was planning to take the month of May off to visit. But then the PRP threw a new kink into things since the timing is different from what we’d been doing before. So, where I’ve landed is that I’ll do PRP and then go to Utah in the next 4 weeks afterwards. Once the PRP is done, we just let things “brew” as the IVF coordinator relayed to me. And I don’t have to go in for bloodwork and ultrasounds in those 4 weeks. Then, once I get back from Utah, I’ll resume my twice-weekly appointments at the clinic.
I feel good, although tired like I was in month 1. I’m also having problems sleeping again, but both of those things are manageable. And yes, I did get to go to the Masters so at least fertility stuff didn’t prevent that. 🙂
—
Note: Like I’ve shared in my previous posts on the topic, I’m not a doctor and I’m not in the medical field so I may get little details wrong and everyone’s experience will be different since the treatment and protocols are unique to each situation. There is no one size fits all. So don’t take any of this as medical advice or as an indication that your process will be exactly the same.
Also, if you decide to leave a comment, please be kind. This is a hard, sensitive time for Tommy and me but I truly do hope that sharing our experience can help others. I’ve received a number of messages on Instagram telling me that it has helped others feel less alone. And hearing from YOU has also made me feel less alone. So thank you for sharing your struggles with me as well.


Leave a Comment
12 responses to “Month 3 of Fertility Treatments: Gonal F Protocol”
I am sure you know but there is another clinic in Charlotte called REACH-Reproductive Endocrinologists of Charlotte if you’re looking for other options.
I haven’t heard of that one – thank you! It’s hard to think about traveling 90+ minutes for appointments every 2-3 days, but I may get to that point!
You are the bravest EVER.
Just wondering if anyone has suggested you try a natural cycle transfer? Has anyone monitored your lining on a non medicated cycle? Sorry if it’s annoying question and you’ve already tried it. I just thought since you’re saying the communication and treatment options at your clinic are frustrating, they may not have raised it. Some clinics don’t love natural cycle transfers because they are more time intensive, unpredictable and require more monitoring.
Actually NO, that hasn’t come up! That is a great question I should ask the clinic. I think they measured my lining for a full cycle in January so maybe we have that baseline… I can’t remember. But I’m going to ask about that. Thank you so much!
Ew. I am angry and frustrated for you about the awful lack of communication you’re having with your clinic. That’s not acceptable at all and I hope this is a front desk issue and not something the Dr is telling them to do. Definitely talk to him and get your answers! Also re: another clinic – a lot of them will let you do remote monitoring at a local place in case you can’t commute that much or that far and you just go there for the actual transfer or procedure! Something to think about if things don’t get better ??. The wait is so, so hard ??
As mentioned above, REACH is an option. Carolina Fertility Institute, also in Charlotte, is another option. While not local to you, each of my friends who used them have had a healthy pregnancy!
Praying so hard for you and your sweet fam, friend.??
I’m sorry you are not having a desirable experience at CFI, I too had an awful experience with them last year and never went back. I hate you also had a bad experience with Baptist because I had a great experience there. You are so brave and strong to continue trying but that’s what moms do, they never give up when it comes to their babies! ??
I so admire your vulnerability on such a sensitive topic. I am sure there are people suffering in the dark about so many of the topics you experience.
you sharing your story helps them feel seen.
You are a light for us to feel less alone.
Also, as a health care professional, it is reasonable for you to ask about a procedure, success rate, precautions, etc before receiving it.
The actual doctor probably has no problem answering your question, but the front office/support staff often does not have a medical background themselves. to answer complicated medical questions.
I am praying for your journey and the tender hearts of your beautiful family.
Fertility treatments are the pits. I love you. You’re brave. You’re smart. And you can do this. Xoxo
Almost twenty years and two adoptions later, infertility is still a trigger for me. It shouldn’t – I have the BEST children through the gift of adoptions – but I can still feel grief, guilt, jealousy, and failure around my infertility. Wishing you grace and peace in your journey. This is hard stuff.